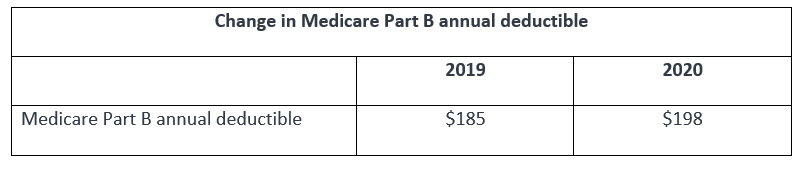
Medicare Part B will probably handle the billing for that clinic visit because it’s typically an outpatient service. Medicare Part B also employs a deductible. Unlike Part A, Part B has an annual deductible. In 2019, the annual Part B deductible is $185. Per-episode deductibles are less common than annual deductibles, although as noted above, Medicare Part A assesses deductibles based on benefit periods rather than calendar years, so it's possible to have to pay the deductible more than once in a given Conversely, the Medicare A system also ensures that if you're hospitalized in December and remain hospitalized into January, you'll.
Yes, we could collect the payment but it has to be refunded promptly if you are collecting excess payment or collected incorrectly. See the below what says in Medicare contract.Yes its a good practice too improve patient payment collection.
Provider Refunds to Beneficiaries
In the agreement between CMS and a provider, the provider agrees to refund as promptly as possible any money incorrectly collected from Medicare beneficiaries or from someone on their behalf.
Money incorrectly collected means any amount for covered services that is greater than the amount for which the beneficiary is liable because of the deductible and coinsurance requirements.
Amounts are considered to have been incorrectly collected because the provider believed the beneficiary was not entitled to Medicare benefits but:
• The beneficiary was later determined to have been entitled to Medicare benefits;
• The beneficiary’s entitlement period fell within the time the provider’s agreement with CMS was in effect; and
• Such amounts exceed the beneficiary’s deductible, coinsurance or non covered services liability.
Requiring Prepayment as a Condition of Admission is Prohibited
Providers must not require advance payment of the inpatient deductible or coinsurance as a condition of admission. Additionally, providers may not require that the beneficiary prepay any Part B charges as a condition of admission, except where prepayment from non-Medicare patients is required. In such cases, only the deductible and coinsurance may be collected.
When Prepayment May Be Requested
he provider may collect deductible or coinsurance amounts only where it appears that the patient will owe deductible or coinsurance amounts and where it is routine and
customary policy to request similar prepayment from non-Medicare patients with similar benefits that leave patients responsible for a part of the cost of their hospital services. In admitting or registering patients, the provider must ascertain whether beneficiaries have medical insurance coverage. Where beneficiaries have medical insurance coverage, the provider asks the beneficiary if he/she has a Medicare Summary Notice (MSN) showing his/her deductible status. If a beneficiary shows that the Part B deductible is met, the provider will not request or require prepayment of the deductible.
Except in rare cases where prepayment may be required, any request for payment must be made as a request and without undue pressure. The beneficiary (and the beneficiary’s family) must not be given cause to fear that admission or treatment will be denied for failure to make the advance payment.
Providers must insure that the admitting office personnel are informed and kept fully aware of the policy on prepayment. For this purpose, and for the benefit of the provider and the public, it is desirable that a notice be posted prominently in the admitting office or lobby to the effect that no patient will be refused admission for inability to make an advance payment or deposit if Medicare is expected to pay the hospital costs.
Guide for Patient
What you pay
For most services, you (or your supplemental coverage) pay the following:
• The yearly Part B deductible if you haven’t already paid it for the year.
• A copayment amount for each service you get in an outpatient visit. For each service, this amount generally can’t be more than the Part A inpatient hospital
deductible. If you get hospital outpatient services in a critical access hospital, your copayment may be higher and may exceed the Part A hospital stay deductible.
• All charges for items or services that Medicare doesn’t cover.
Example: Mr. Davis needs to have his cast removed. He goes to his local hospital outpatient department. The hospital charges $150 for this procedure. His copayment amount for this procedure, under the outpatient prospective payment system, is $20. Mr. Davis has paid $85 of his $155 Part B deductible. To have his cast removed, Mr. Davis must pay $90 ($70 remaining deductible amount + $20 copayment amount).
The amount you pay may change each year. The amount you pay may also be different for different hospitals.
Note: If you have a Medigap (Medicare Supplement Insurance) policy, other supplemental coverage, or employer or union coverage, it may pay the Part B deductible and copayment amounts.
If you paid more than the amount listed on your Medicare Summary Notice
 After Medicare gets a bill from the hospital, you will get a Medicare Summary Notice. This notice will show how much you have to pay for the services you got. It will also show how much Medicare paid the hospital for the services. If the amount you paid the hospital or community mental health center at the time of service is more than what was listed on the Medicare Summary Notice, call the provider and ask for a refund. Tell them you paid more than the amount listed on the Medicare Summary Notice.
After Medicare gets a bill from the hospital, you will get a Medicare Summary Notice. This notice will show how much you have to pay for the services you got. It will also show how much Medicare paid the hospital for the services. If the amount you paid the hospital or community mental health center at the time of service is more than what was listed on the Medicare Summary Notice, call the provider and ask for a refund. Tell them you paid more than the amount listed on the Medicare Summary Notice.If you paid less than the amount listed on your Medicare Summary Notice
If you paid less than the amount listed on your Medicare Summary Notice, the hospital or community mental health center may bill you for the difference if you don’t have another insurer who is responsible for paying your deductible and copayments.
MEDICAID DEDUCTIBLE BENEFICIARIES AND MSP
Beneficiaries may be a MSP and also a Medicaid deductible beneficiary. The beneficiary will have a Benefit Plan ID of QMB until the deductible amount has been met. The Benefit Plan ID will change to MA once the deductible amount is met. For this Medicaid eligibility period, Medicaid reimburses the provider for Medicaid-covered services, as well as the Medicare coinsurance and deductible amounts up to the Medicaid allowable.
If Medicare covers the service, the provider may bill Medicaid for the coinsurance and deductible amounts only. For any Medicare noncovered services, the beneficiary should obtain proof of the incurred medical expense to present to the MDHHS worker so the amount may be applied toward the beneficiary's Medicaid deductible amount.
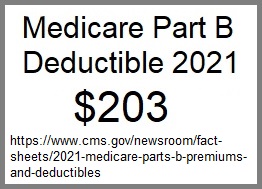
What is the Medicare Part B deductible for 2021?
In 2021, the Medicare Part B deductible is $203 per year.
What is the Medicare Part A deductible for 2021?
The Medicare Part A deductible for 2021 is $1,484 per benefit period.
Yearly Deductible For Medicare Part A
Unlike the deductible for Part B that operates on an annual basis, the Part A deductible starts and stops with each benefit period.
A benefit period begins the day you are admitted for inpatient care at a hospital or skilled nursing facility, and it ends when you have gone 60 consecutive days without inpatient treatment.
For example, if you are admitted for inpatient hospital care on June 1 and are discharged on June 10, you would still be in the same benefit period if you were admitted again for inpatient care on June 30. You wouldn't have to meet your Part A deductible again if you already met that deductible during your first hospital stay.
If, however, you were discharged on June 10 and were readmitted to the hospital in October of the same year, you would be in a new benefit period. Game dev tycoon trainer. You would need to meet the Part A deductible again before your Medicare Part A coverage would kick in again.
Is there a deductible with Medicare?
Yes, both Medicare Part A and Medicare Part B each come with a deductible.
Medicare Advantage (Part C) and Medicare Prescription Drug Plans (Part D) may also include deductibles as well, although the costs associated with these plans are not standardized like they are in Original Medicare (Part A and Part B). Some Part D plans include $0 deductibles before the plan's drug coverage kicks in.
Medicare defines a deductible as:
“The amount you must pay for health care or prescriptions before Original Medicare, your prescription drug plan, or your other insurance begins to pay.”
In other words, a deductible is the amount that you must first pay out of your own pocket for health care before your Medicare insurance coverage kicks in.
What counts toward the Medicare Part B deductible?
Basically, any service or item that is covered by Part B counts toward your Part B deductible.
Yearly Deductible For Medicare 2021
For example, imagine you fall and break your leg. You are taken to a hospital, treated, and released with a pair of crutches.
The care you receive as a hospital inpatient is covered under Medicare Part A (hospital insurance). But the crutches are covered under Medicare Part B (medical insurance).
The amount that you are charged for the doctor, treatment, and the crutches will count toward your Part B deductible, while the bill for your hospital stay will count toward your Part A deductible.
Each part of Medicare carries its own deductible. The Part A and Part B deductibles are standard for each beneficiary of Original Medicare.
The Part C (Medicare Advantage) and Part D (prescription drug plan) deductibles will vary from plan to plan. Some Part C and Part D plans may have a $0 deductible.
Some Medicare Advantage plans also feature $0 premiums, and most plans offer drug coverage and may offer routine dental and vision benefits. Call to speak with a licensed insurance agent who can help you compare plans and – if you're eligible – help you enroll in a new plan, right from the comfort of your own home.
You can also compare plans online for free, with no obligation to enroll.
Or call 1-800-557-60591-800-557-6059TTY Users: 711 to speak with a licensed insurance agent. We accept calls 24/7!
What happens once you reach the deductible?
Once you meet the required Medicare Part B deductible, you will typically be charged a 20 percent coinsurance for all Part B-covered services and items for the remainder of the year.
Coinsurance is the amount of the total bill that you must pay. A 20 percent coinsurance means you (the beneficiary) would be responsible for 20 percent of a medical bill, while Medicare would pay the remaining 80 percent.
It’s worth noting that the 20 percent you will pay as coinsurance is 20 percent of the Medicare-approved amount.
The Medicare-approved amount is the maximum amount that a health care provider is allowed to charge for a service or item as determined by Medicare.
Let’s use the broken leg scenario from above and say that the cost of the pair of crutches was $80.
- If the injury happened before reaching your Medicare Part B deductible, you would be responsible for the full $80 (or the amount it would require you to reach $203 in covered spending for the year in 2021).
- If you had already met the Part B deductible prior to the injury happening in this hypothetical situation, you would only be responsible for $16 (20 percent of $80). Medicare would then pay the remaining $64.
What was the Medicare Part B deductible for 2020?
In 2020, the Medicare Part B Deductible was $198 per year.
As mentioned above, the 2021 Medicare Part B deductible is $203 per year.
Below is a look at how the Part B deductible has increased (and in one case, decreased) since 2008.
| 2008 | $135 |
| 2009 | $135 |
| 2010 | $155 |
| 2011 | $162 |
| 2012 | $140 |
| 2013 | $147 |
| 2014 | $147 |
| 2015 | $147 |
| 2016 | $166 |
| 2017 | $183 |
| 2018 | $183 |
| 2019 | $185 |
| 2020 | $198 |
| 2021 | $203 |
Is there a way to avoid paying the Medicare Part B deductible?
There are two ways you may be able to avoid having to pay the Medicare Part B deductible:
- Medicare Supplement Insurance
Medicare Supplement Insurance (also called Medigap) is a type of privately-sold insurance plan that is used in conjunction with Medicare Part A and Part B.
Medigap plans help provide coverage for some of the out-of-pocket expenses that Medicare beneficiaries are responsible for paying, such as Medicare coinsurance and deductibles.
There are two Medicare Supplement Insurance plans (Plan F and Plan C) that cover 100 percent of the Medicare Part B deductible. If you enroll in one of these types of plans and pay a monthly premium to belong to the plan, you will not have to pay out of your own pocket for the Medicare Part B deductible.
It's important to note that Plan F and Plan C are no longer available for new Medicare beneficiaries who became eligible for Medicare after January 1, 2020.
If you became eligible for Medicare before that date, you may still be able to enroll in either plan if they are available where you live. If you already had Plan C or Plan F before January 1, 2020, you can keep your plan.
Most of the 10 standardized types of Medigap plans available in most states provide partial or full coverage of the Part A deductible. - Medicare Advantage
Enrolling in a Medicare Part C plan (also called a Medicare Advantage plan) is another way of avoiding the Part B deductible.
It's important to note that Medicare Part C is a term only used for Medicare Advantage plans, and it's not the same as Medigap Plan C.
Medicare Advantage plans provide the same benefits as Medicare Part A and Part B in one plan and serve as an alternative way to get Original Medicare coverage.
Many Medicare Advantage plans may also offer some additional benefits not covered by Medicare Part A and Part B.
Medicare Advantage plans may have their own deductible, but you will not be responsible for the Medicare Part B deductible if you are enrolled in a Medicare Advantage plan. You will only be responsible for paying your Medicare Advantage plan deductible.
As mentioned above, some Medicare Advantage plans have no deductible, and some plans even offer $0 monthly premiums.
Explore your Medicare enrollment options
If you have further questions about the Medicare Part B deductible or any other costs associated with Medicare, explore our guide to Medicare costs.
Learn more about your Medicare enrollment options. If you want to have Medicare health coverage without having to pay the Medicare Part B deductible, you may want to consider enrolling in a Medicare Advantage plan.
Call today to speak with a licensed insurance agent to find the right plan for your needs.
Find Medicare Advantage plans in your area
Or call 1-800-557-60591-800-557-6059TTY Users: 711 to speak with a licensed insurance agent. We accept calls 24/7!
